Capillary blood sampling is one of two microsampling approaches used within dried blood spot (DBS) testing today. In contrast to standard blood testing, where specialised needles are used to remove blood directly from veins (i.e. venous blood draws), capillary-based microsampling uses a specially-designed lancet to prick the skin on a heel, fingertip, or other collection site on the body, to draw small amounts of blood in the 10 to 50 microlitre range from the capillaries (tiny blood vessels near the surface of the skin) in a quick and non-invasive manner.
Besides the increased patient comfort that may come with capillary testing, capillary blood samples are often easier to obtain than venous blood, especially in infants or individuals with difficult or damaged veins (as a result of regular testing). The simplicity of capillary blood sampling also makes it ideal for home testing in certain situations as the procedure requires minimal training, making it an attractive option in remote areas or for individuals who find it difficult to attend medical facilities for venous blood testing.
This blog post looks at three parameters that should be considered before performing capillary blood sampling, and provides practical tips to help achieve sampling success.
1. Choice of collection site
An additional advantage of capillary blood sampling over venepuncture is that several collection sites on the body may be used for sampling, and these sites can be rotated to avoid scarring. The primarily used collection sites are the fingertip and heel, although the ear lobe, big toe and palm of the hand may be used in special circumstances where other collection sites are unavailable/unsuitable, or in certain patient groups.
Although no international standards exist for capillary blood sampling, the World Health Organisation (WHO) guidelines on drawing blood recommends that the collection site for capillary blood sampling in infants and children is determined by the patient’s age and weight (1). The heel is almost exclusively used to take samples for newborn screening programmes, while the fingertip is usually the preferred site for capillary blood testing in children and adults. For infants who have learned to walk, the fingertip is a more suitable collection site than the heel since walking may lead to callus formation, which may prevent adequate blood flow. If for some reason fingertip sampling can not be performed in a young child who is walking, the big toe may be used.
Once the collection site has been chosen, the following factors can be taken into account to maximise the likelihood of sampling success while minimising the risk of pain and scarring:
- For fingertip sampling: it is recommended to use the middle or fourth finger of the non-dominant hand (2). The thumb has a pulse and may bleed excessively, while the second (index) and fifth (little) fingers are often less suitable because of hardened skin and reduced tissue content, respectively. Puncturing is ideally performed across the lines of the fingerprint to ensure that the blood wells up into a large rounded drop (2). Always choose a position on the left or right side of the fingertip as these areas contain fewer nerve endings than the centre of the fingertip, thus reducing pain or discomfort. For regular testing, it is wise to rotate sampling sites on the sides of the fingertips to avoid callus formation due to repeatedly puncturing the same site.
- For heel-prick sampling: in non-walking infants up to approximately 1 year old (or maximum weight 10 kg), the recommended puncture site is the medial or lateral plantar surface (i.e. the sides) of the heel (3). Note that punctures performed on the plantar surface of the foot can damage cartilage or bone. Studies have found that heel-prick testing can be more painful for newborns than venepucture, thus pain relief is recommended when performing heel prick in this group (3,4). Suitable pain relief and soothing measures include breastfeeding, skin-to-skin contact, and swaddling combined with holding the baby upright. Sucrose and pacifiers may also be used to manage pain during the procedure (3).
The fingertip is the most common capillary blood sampling site in adults. The safety lancet makes the fingerprich easy and standardised with regard to size and depth.
2. Control the flow – lancet type and design
Choosing a lancet of suitable length and depth is critical to obtaining a useful sample while minimising patient discomfort. The WHO recommends using a lancet that is slightly shorter than the estimated depth needed because the pressure compresses the skin; thus, the actual puncture depth will be slightly deeper than the lancet length (1). Lancet lengths vary across manufacturers, and typically range from 0.85 mm (for newborn babies) up to 2.2 mm for adults. For heel-prick samples from full-term newborns, the lancet depth should not go beyond 2.4 mm. For premature neonates, a 0.85 mm lancet should be used (1).
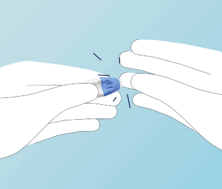
Nowadays, safety lancets are widely used for capillary sampling. These are sterile, single-use products in which the blade or needle is automatically retracted into the lancet cover after puncture. This helps to prevent injury and contamination, as well as facilitating safer disposal of used lancets. There are many different types of safety lancets available, typically covering a range of puncture depths from 1 to 2 mm.
3. Optimise the local conditions
Although this blog post should not replace a detailed sampling procedure for capillary blood sampling, the following tips should maximise the chances of obtaining a useful sample.
- Warm the site. Capillary blood samples are always best obtained when the collection site is warm. For fingertip testing, it is recommended to warm the hands up by rubbing, while heel testing in babies is most successful when the baby is warm.
- Clean collection site. To avoid sample contamination or infection by local microflora, the collection site should always been cleaned before puncture by wiping with a suitable alcohol solution followed by air drying.
- Only use the lancet and puncture site once. To avoid sample contamination or infection caused by transferring skin microflora from one site to another, a lancet and a single puncture site should only ever be used once.
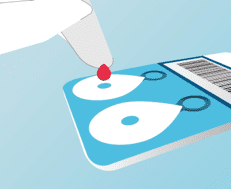
- Discard the first drop of blood. Once a site has been punctured and blood is flowing, the first drop of blood must always be discarded, since this contains tissue fluid that can contaminate the blood sample and skew test results (3).
- Don’t milk the site! While gently rubbing around a collection site to warm up the area can improve the chances of successful sampling, it is critical not to strongly squeeze or ‘milk’ the site or to vigorously agitate the sample after collection, as this can destroy the red blood cells and interfere with downstream assay reliability (3).
In this blog post, we have shared considerations and tips that may help when performing capillary testing, as a supplement to a well-tested procotol. To learn more, you may access Capitainer’s Instructions for Use recommended capillary sampling procedure for our microsampling capillary device Capitainer®B here.
To the Capitainer®B device, one single drop capillary blood is added to the sample inlet of the card, producing a quantitative dried blood spot, protected from contamination within the device.